Thursday, September 10, 2009
Day 1 of Living with GD
I got my Glucometer and was shown how to do it. We did my first test in the office at 1:25pm which was 3 hours after I ate a bowl of Rice Crispies my number was 115 which she stated was too high I should be at a fasting number at that point which is under 90
UGH!
"Eat your lunch and from the moment of your first bit note the time and test 2 hours later your number should not be over 120" she tells me
Afraid to eat! What do I eat??
.....am sooo hungry but have a 40 min drive home. Oh well lets see what I can do at McDonalds
I order a cheeseburger, small fry and Fruit Walnut Salad
I have water Bottle with me.....fries just arent the same without soda or tea!
First Bite 1:55pm
I eat the cheeseburger, fries and half of the fruit and walnut salad
Second test 3:55pm I can do this laid everything out am ready to go
STICK!
Placed the blood on the strip BEEP
a few seconds later my number is......120! Whew! Just made it on that one.
But now its time for a snack.....UGH! Another thing to find and not really want
Cucumber Salad it is.....sure wish it was some chips!
2 more hours til dinner and 4 more til I have to test again.....til then
Got the Call!
During and After the test I was sooo sick I was lethargic, dizzy, and did not want to eat
Yesterday, I Got the Call!
"Hi Ms Anderson its Rita from the Doctors office I have your results of your Glucose and Unfortunately..."
"Stop right there" I said "dont tell me!"
"I am sorry but you failed"Rita says
I asked her for my numbers and they were as follows:
Fasting 88
1 hour 181 (fail)
2 hour 116
3 hour 146 (fail)
"Because you failed 2 out of 4 you must now go to the Diabetic Counselor and Nutritionist.
They will guide you on diet, using the glucometer etc...."
I said "Wait you mean I have to stick myself?"
Rita says "Yes unfortunately, if they dont call you by the end of today call me in the morning because you need to be seen right away"
I said "Ok great thanks for calling"
Of course I then start googling everything I could find on Gestational Diabetes and found that there can be some serious consequences if I can keep this controlled for both me and my Baby Girl.
Some of what I found is below:
Effects of Stress on Sugar & Insulin Levels
Stress Increases Your Sugar and Insulin Levels thats a fact
Under stress your body triggers a state of alarm–the primitive ” flight or fight ” response. The adrenal glands ( small glands that sit on top of your kidneys) release stress hormones ( cortisol & adrenalin) into the bloodstream under stress. Theis response also increases the levels of fat, sugar and insulin in your blood. This is to prepare you for increased energy needs to perform your ” flight or fight” response.
You are having a busy day, no time for lunch and are grabbing all those high sugar/carbohydrate snacks-your sugar & insulin levels are really high and you are really riding that viscious roller coaster.You cant even imagine that you could possibly be gaining weight-but you are!! You can diet, think you are increasing the amount of energy you burn up and gain weight at the same time if you are under stress. This weight gain is due to the body`s original design to protect itself at all costs.
This also leads to insulin resistance:
Stress doesn`t even have to be real…it can be perceived.
Some of the causes of stress are: depression, anxiety, grief, low socioeconomic status, divorce, lonliness, unemployment, exposure to cold, environmental toxins, pain, too much exercise, smoking, stimulants, infection and being overweight.
Sleep deprivation is a major source of stress today and a major contributor to hunger and craving for high carbohydrate sugary foods.
High levels of cortisol and adrenalin can become a chronic condition leading to depression, memory loss, bone loss, heart disease, cancer and immune diseases.
Under stress the sympathetic nervous system gets turned on causing increased hunger, slow metabolism, increased blood sugar, heartburn or reflux and constipation. The stress hormone, cortisol, causes you to become less sensitive to `leptin`-the hormone that tells your brain you are full and therefore you keep eating and eating under stress.
Digestion is very poor under stress and you wont get the nutrients from your food.
Higher levels of cortisol also cause low levels of testosterone and thyroid hormones.
Cortisol normally rises in the morning increasing your appetite so you will eat breakfast and have energy for the day. Cortisol then decreases in the evening and growth hormone and melatonin levels rise to prepare you for sleep and boby repair. Under stress this rhythm is disrupted causing some people to have `night-eating syndrome`. This condition leads to a decrease in appetite in the morning and increased hunger at night.
How to reduce stress:
Identify & try to reduce the causes of stress
Correct your insulin resistance using the all natural supplement `Glucofast`
Learn active relaxation exercises
Learn & practice deep breathing for relaxation–breathe in deeply, exhale slowly while commanding your body to relax, breath in deeply, exhale-relax. Repeat…Do anytime, anywhere even for a few minutes.
Eat whole foods that reduce stress ie: green leafy vegetables, high antioxidant fruits, whole grains, omega 3`s from wild fish or ground flaxseeds and lots of fiber.
Supplements:
Antioxidants-vitamin C & E, zinc, B-complex, coenzyme Q10 and lipoic acid.
Potassium & Magnesium help balance the adrenals
Herbs can help you adapt to stress-ginseng, rhodiola, ashwagandha and licorice.
Managing stress in your life can make huge improvements in your overall health.
INTRO
You are 28-30 weeks pregnant.
Your health care provider has just told you that you have gestational diabetes.
Should you be concerned about gestational diabetes?
The short answer:
YES! Good care means a lot for your health and your baby’s health.
What is gestational diabetes?
Pregnant women who have never had diabetes before but who have high blood sugar (glucose) levels during pregnancy are said to have gestational diabetes. Gestational diabetes affects about 4% of all pregnant women - about 135,000 cases of gestational diabetes in the United States each year.
We don’t know what causes gestational diabetes, but we have some clues. The placenta supports the baby as it grows. Hormones from the placenta help the baby develop. But these hormones also block the action of the mother’s insulin in her body. This problem is called insulin resistance. Insulin resistance makes it hard for the mother’s body to use insulin. She may need up to three times as much insulin.
Gestational diabetes starts when your body is not able to make and use all the insulin it needs for pregnancy. Without enough insulin, glucose cannot leave the blood and be changed to energy. Glucose builds up in the blood to high levels. This is called hyperglycemia.
How gestational diabetes can affect your baby?
Gestational diabetes affects the mother in late pregnancy, after the baby’s body has been formed, but while the baby is busy growing. Because of this, gestational diabetes does not cause the kinds of birth defects sometimes seen in babies whose mothers had diabetes before pregnancy.
However, untreated or poorly controlled gestational diabetes can hurt your baby. When you have gestational diabetes, your pancreas works overtime to produce insulin, but the insulin does not lower your blood glucose levels. Although insulin does not cross the placenta, glucose and other nutrients do. So extra blood glucose goes through the placenta, giving the baby high blood glucose levels. This causes the baby’s pancreas to make extra insulin to get rid of the blood glucose. Since the baby is getting more energy than it needs to grow and develop, the extra energy is stored as fat.
This can lead to macrosomia, or a “fat” baby. Babies with macrosomia face health problems of their own, including damage to their shoulders during birth. Because of the extra insulin made by the baby’s pancreas, newborns may have very low blood glucose levels at birth and are also at higher risk for breathing problems. Babies with excess insulin become children who are at risk for obesity and adults who are at risk for type 2 diabetes.
Treating gestational diabetes
Because gestational diabetes can hurt you and your baby, you need to start treatment quickly. Treatment for gestational diabetes aims to keep blood glucose levels equal to those of pregnant women who don’t have gestational diabetes. Treatment for gestational diabetes always includes special meal plans and scheduled physical activity. It may also include daily blood glucose testing and insulin injections. You will need help from your doctor, nurse educator, and other members of your health care team so that your treatment for gestational diabetes can be changed as needed.
For you as the mother-to-be, treatment for gestational diabetes helps lower the risk of a cesarean section birth that very large babies may require. Sticking with your treatment for gestational diabetes will give you a healthy pregnancy and birth, and may help your baby avoid future poor health.
Gestational diabetes — Looking ahead
Gestational diabetes usually goes away after pregnancy. But once you’ve had gestational diabetes, your chances are 2 in 3 that it will return in future pregnancies. In a few women, however, pregnancy uncovers type 1 or type 2 diabetes. It is hard to tell whether these women have gestational diabetes or have just started showing their diabetes during pregnancy. These women will need to continue diabetes treatment after pregnancy.
Many women who have gestational diabetes go on to develop type 2 diabetes years later. There seems to be a link between the tendency to have gestational diabetes and type 2 diabetes. Gestational diabetes and type 2 diabetes both involve insulin resistance. Certain basic lifestyle changes may help prevent diabetes after gestational diabetes.
Losing weight:
Are you more than 20% over your ideal body weight? Losing even a few pounds can help you avoid developing type 2 diabetes.
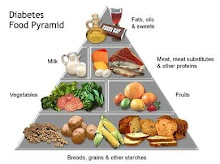
Making healthy food choices:
Follow simple daily guidelines, like eating a variety of foods including fresh fruits and vegetables, limiting fat intake to 30% or less of daily calories, and watching your portion size. Healthy eating habits can go a long way in preventing diabetes and other health problems.
Exercising:
Regular exercise allows your body to use glucose without extra insulin. This helps combat insulin resistance and is what makes exercise helpful to people with diabetes. Never start an exercise program without checking with your doctor first.
Keeping worry in perspective:
While gestational diabetes is a cause for concern, the good news is that you and your health care team - your doctor, obstetrician, nurse educator, and dietitian - work together to lower your high blood glucose levels. And with this help, you can turn your concern into a healthy pregnancy for you, and a healthy start for your baby.